Evaluation of the Effects of Anastomosis Angle on the Performance of an Optimized Spiral Flow-Inducing Graft Design using CFD
DOI:
https://doi.org/10.37934/cfdl.15.11.118130Keywords:
Bypass Graft, Spiral Flow, Anastomosis Angle, Hemodynamics, Computational Fluid Dynamics (CFD)Abstract
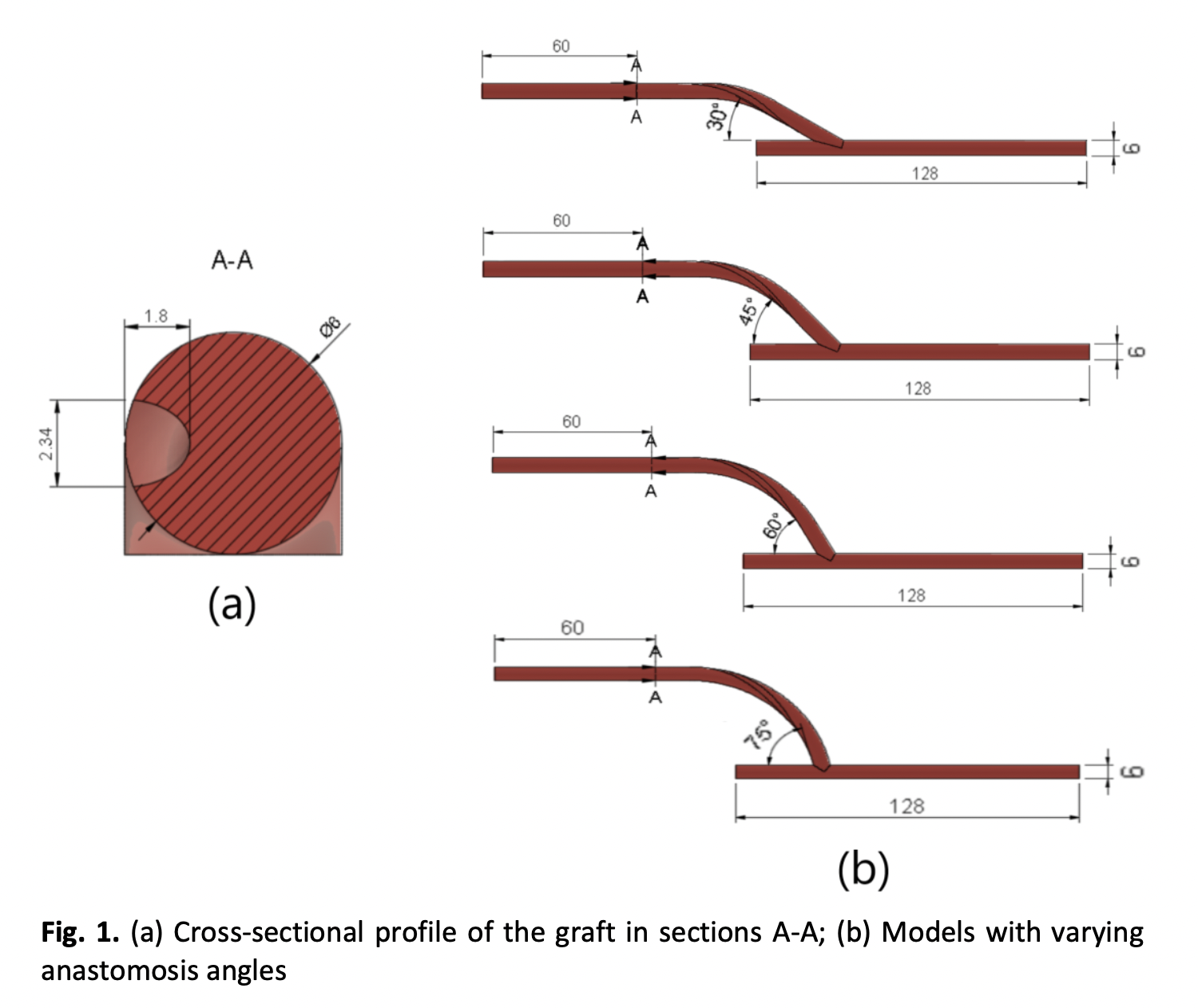
Bypass grafting is a common medical intervention used for people suffering from atherosclerosis, but the prevalence of graft failure due to disturbed hemodynamics necessitates the improvement of graft design for optimum blood flow. Spiral flow has been proposed as a mechanism to improve hemodynamics in grafts. A previous study optimized a spiral flow-inducing graft design, but it did not consider the effects of anastomosis angle despite its significant effects on blood flow. The purpose of this research is to further enhance the performance and patency of bypass grafts by determining how the anastomosis angle affects the hemodynamics of a spiral flow-inducing graft design using computational fluid dynamics (CFD). Distal anastomoses of 6 mm ridged graft and femoral artery constructs at varying anastomosis angles of 15° increments were analysed using steady-state CFD analysis under the assumptions of laminar, isothermal, stationary, rigid, non-Newtonian, and incompressible flow to determine the anastomosis angle that would yield optimum flow parameters. A 30° anastomosis angle was found to yield the most favourable flow conditions, particularly by minimizing recirculation one millimetre and five millimetres away from the toe (0.26% and 0% of the cross-sectional area of the artery, respectively) and pressure drop (474.8 Pa), as well as the complete elimination of areas affected by pathologically high wall shear stress (WSS). The findings of this study point out the potential benefits of a smaller anastomosis angle on the performance and patency of bypass grafts through the minimization of pressure drop and areas affected by recirculation and abnormally high WSS.
Downloads
References
Kaptoge, Stephen, Lisa Pennells, Dirk De Bacquer, Marie Therese Cooney, Maryam Kavousi, Gretchen Stevens, Leanne Margaret Riley et al., "World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions." The Lancet global health 7, no. 10 (2019): e1332-e1345.
Aaronson, Philip I., Jeremy PT Ward, and Michelle J. Connolly. The cardiovascular system at a glance. John Wiley & Sons, 2020.
Subramaniam, Thineshwaran, and Mohammad Rasidi Rasani. "Pulsatile CFD Numerical Simulation to investigate the effect of various degree and position of stenosis on carotid artery hemodynamics." Journal of Advanced Research in Applied Sciences and Engineering Technology 26, no. 2 (2022): 29-40. https://doi.org/10.37934/araset.26.2.2940
Pashneh-Tala, Samand, Sheila MacNeil, and Frederik Claeyssens. "The tissue-engineered vascular graft—past, present, and future." Tissue Engineering Part B: Reviews 22, no. 1 (2016): 68-100. https://doi.org/10.1089/ten.teb.2015.0100
Zhang, Fan, Tushar Bambharoliya, Yu Xie, Laijun Liu, Hakan Celik, Lu Wang, Ozan Akkus, and Martin W. King. "A hybrid vascular graft harnessing the superior mechanical properties of synthetic fibers and the biological performance of collagen filaments." Materials Science and Engineering: C 118 (2021): 111418. https://doi.org/10.1016/j.msec.2020.111418
Elliott, Morgan B., Brian Ginn, Takuma Fukunishi, Djahida Bedja, Abhilash Suresh, Theresa Chen, Takahiro Inoue et al., "Regenerative and durable small-diameter graft as an arterial conduit." Proceedings of the National Academy of Sciences 116, no. 26 (2019): 12710-12719. https://doi.org/10.1073/pnas.1905966116
Fan, Yubo, Zaipin Xu, Wentao Jiang, Xiaoyan Deng, Ke Wang, and Anqiang Sun. "An S-type bypass can improve the hemodynamics in the bypassed arteries and suppress intimal hyperplasia along the host artery floor." Journal of biomechanics 41, no. 11 (2008): 2498-2505. https://doi.org/10.1016/j.jbiomech.2008.05.008
Arefin, Md Shamsul. "Hemodynamic and structural effects on bypass graft for different levels of stenosis using fluid structure interaction: A prospective analysis." Journal of Vascular Nursing 37, no. 3 (2019): 169-187. https://doi.org/10.1016/j.jvn.2019.05.006
Donadoni, Francesca, Cesar Pichardo-Almarza, Shervanthi Homer-Vanniasinkam, Alan Dardik, and Vanessa Díaz-Zuccarini. "Multiscale, patient-specific computational fluid dynamics models predict formation of neointimal hyperplasia in saphenous vein grafts." Journal of Vascular Surgery Cases, Innovations and Techniques 6, no. 2 (2020): 292-306. https://doi.org/10.1016/j.jvscit.2019.09.009
Hajati, Omid, Khalil Zarrabi, Reza Karimi, and Azadeh Hajati. "CFD simulation of hemodynamics in sequential and individual coronary bypass grafts based on multislice CT scan datasets." In 2012 annual international conference of the IEEE engineering in medicine and biology society, pp. 641-644. IEEE, 2012. https://doi.org/10.1109/EMBC.2012.6346013
Dur, Onur, Sinan Tolga Coskun, Kasim Oguz Coskun, David Frakes, Levent Burak Kara, and Kerem Pekkan. "Computer-aided patient-specific coronary artery graft design improvements using CFD coupled shape optimizer." Cardiovascular engineering and technology 2 (2011): 35-47. https://doi.org/10.1007/s13239-010-0029-z
Khader, Shah Mohammed Abdul, Adi Azriff, Cherian Johny, Raghuvir Pai, Mohammad Zuber, Kamarul Arifin Ahmad, and Zanuldin Ahmad. "Haemodynamics behaviour in normal and stenosed renal artery using computational fluid dynamics." Journal of Advanced Research in Fluid Mechanics and Thermal Sciences 51, no. 1 (2018): 80-90.
Ningappa, Abhilash Hebbandi, Suraj Patil, Gowrava Shenoy Belur, Augustine Benjamin Valerian Barboza, Nitesh Kumar, Raghuvir Pai Ballambat, Adi Azriff Basri, Shah Mohammed Abdul Khader, and Masaaki Tamagawa. "Influence of altered pressures on flow dynamics in carotid bifurcation system using numerical methods." Journal of Advanced Research in Fluid Mechanics and Thermal Sciences 97, no. 1 (2022): 47-61. https://doi.org/10.37934/arfmts.97.1.4761
Williams, Dillon, Eric C. Leuthardt, Guy M. Genin, and Mohamed Zayed. "Tailoring of arteriovenous graft-to-vein anastomosis angle to attenuate pathological flow fields." Scientific reports 11, no. 1 (2021): 12153. https://doi.org/10.1038/s41598-021-90813-3
Yang, Chih-Yu, Ming-Chia Li, Chien-Wen Lan, Wang-Jiun Lee, Chen-Ju Lee, Cheng-Hsueh Wu, Jing-Min Tang et al., "The anastomotic angle of hemodialysis arteriovenous fistula is associated with flow disturbance at the venous stenosis location on angiography." Frontiers in bioengineering and biotechnology 8 (2020): 846. https://doi.org/10.3389/fbioe.2020.00846
Liu, Zhaomiao, Gang Yang, Siqi Nan, Yipeng Qi, Yan Pang, and Yi Shi. "The effect of anastomotic angle and diameter ratio on flow field in the distal end-to-side anastomosis." Proceedings of the Institution of Mechanical Engineers, Part H: Journal of Engineering in Medicine 234, no. 4 (2020): 377-386. https://doi.org/10.1177/0954411919894410
Van Tricht, Ilse, Dirk De Wachter, Jan Tordoir, and Pascal Verdonck. "Comparison of the hemodynamics in 6 mm and 4–7 mm hemodialysis grafts by means of CFD." Journal of Biomechanics 39, no. 2 (2006): 226-236. https://doi.org/10.1016/j.jbiomech.2004.12.003
Sawo, Pamir, Andrew Moufarrej, Marije Sloff, Maarten G. Snoeijs, Tammo Delhaas, Jan HM Tordoir, and Barend ME Mees. "The effect of geometric graft modification on arteriovenous graft patency in haemodialysis patients: a systematic review and meta-analysis." European Journal of Vascular and Endovascular Surgery 60, no. 4 (2020): 568-577. https://doi.org/10.1016/j.ejvs.2020.06.023
Longest, P. Worth, Clement Kleinstreuer, and Joseph P. Archie Jr. "Particle hemodynamics analysis of Miller cuff arterial anastomosis." Journal of vascular surgery 38, no. 6 (2003): 1353-1362. https://doi.org/10.1016/S0741-5214(03)00950-9
Ruiz-Soler, Andres, Foad Kabinejadian, Mark A. Slevin, Paulo J. Bartolo, and Amir Keshmiri. "Optimisation of a novel spiral-inducing bypass graft using computational fluid dynamics." Scientific reports 7, no. 1 (2017): 1865. https://doi.org/10.1038/s41598-017-01930-x
Williams, Dillon, Eric C. Leuthardt, Guy M. Genin, and Mohamed Zayed. "Tailoring of arteriovenous graft-to-vein anastomosis angle to attenuate pathological flow fields." Scientific reports 11, no. 1 (2021): 12153. https://doi.org/10.1038/s41598-021-90813-3
Quanyu, Wu, Liu Xiaojie, Pan Lingjiao, Tao Weige, and Qian Chunqi. "Simulation analysis of blood flow in arteries of the human arm." Biomedical Engineering: Applications, Basis and Communications 29, no. 04 (2017): 1750031. https://doi.org/10.4015/S1016237217500314
Lorente, Sylvie, Mathieu Hautefeuille, and Aczel Sanchez-Cedillo. "The liver, a functionalized vascular structure." Scientific Reports 10, no. 1 (2020): 16194. https://doi.org/10.1038/s41598-020-73208-8
Cengel, Yunus, and John Cimbala. Ebook: Fluid mechanics fundamentals and applications (si units). McGraw Hill, 2013.
Inumaru, Jun, Saburo Hara, and Takeharu Hasegawa. "Future perspective and remarks." In Advances in Power Boilers, pp. 461-478. Elsevier, 2021. https://doi.org/10.1016/B978-0-12-820360-6.00010-2
Idris, Muhammad Syafiq, Irnie Azlin Zakaria, and Wan Azmi Wan Hamzah. "Heat transfer and pressure drop of water based hybrid Al2O3: SiO2 nanofluids in cooling plate of PEMFC." Journal of Advanced Research in Numerical Heat Transfer 4, no. 1 (2021): 1-13. https://doi.org/10.37934/arfmts.88.3.96109
Totorean, A. F., S. I. Bernad, I. C. Hudrea, and R. F. Susan-Resiga. "Competitive flow and anastomosis angle influence on bypass hemodynamics in unsteady flow conditions." In AIP Conference Proceedings, vol. 1863, no. 1. AIP Publishing, 2017. https://doi.org/10.1063/1.4992166
Dutra, Rafael F., Flavia SF Zinani, Luiz AO Rocha, and C. Biserni. "Constructal design of an arterial bypass graft." Heat Transfer 49, no. 7 (2020): 4019-4039. https://doi.org/10.1002/htj.21693
Impiombato, A. N., F. S. F. Zinani, L. A. O. Rocha, and C. Biserni. "Pulsatile flow through an idealized arterial bypass graft: an application of the constructal design method." Journal of the Brazilian Society of Mechanical Sciences and Engineering 43, no. 8 (2021): 370. https://doi.org/10.1007/s40430-021-03048-8
Katritsis, Demosthenes, Lambros Kaiktsis, Andreas Chaniotis, John Pantos, Efstathios P. Efstathopoulos, and Vasilios Marmarelis. "Wall shear stress: theoretical considerations and methods of measurement." Progress in cardiovascular diseases 49, no. 5 (2007): 307-329. https://doi.org/10.1016/j.pcad.2006.11.001
Braga, Sandrina Figueiredo, João Rocha Neves, Joana Ferreira, Celso Carrilho, João Correia Simões, and Amílcar Mesquita. "Neointimal hyperplasia." Portuguese Journal of Cardiac Thoracic and Vascular Surgery 26, no. 3 (2019): 213-217.
Khan, Muhammad Owais, Justin S. Tran, Han Zhu, Jack Boyd, René R. Sevag Packard, Ronald P. Karlsberg, Andrew M. Kahn, and Alison L. Marsden. "Low wall shear stress is associated with saphenous vein graft stenosis in patients with coronary artery bypass grafting." Journal of cardiovascular translational research 14 (2021): 770-781. https://doi.org/10.1007/s12265-020-09982-7
Binns, Richard L., David N. Ku, Mark T. Stewart, Joseph P. Ansley, and Kellie A. Coyle. "Optimal graft diameter: effect of wall shear stress on vascular healing." Journal of vascular surgery 10, no. 3 (1989): 326-337. https://doi.org/10.1016/0741-5214(89)90449-7
Hathcock, James J. "Flow effects on coagulation and thrombosis." Arteriosclerosis, thrombosis, and vascular biology 26, no. 8 (2006): 1729-1737. https://doi.org/10.1161/01.ATV.0000229658.76797.30
Malek, Adel M., Seth L. Alper, and Seigo Izumo. "Hemodynamic shear stress and its role in atherosclerosis." Jama 282, no. 21 (1999): 2035-2042. https://doi.org/10.1001/jama.282.21.2035
Malik, J., V. Tuka, and V. Tesař. "Local hemodynamics of the vascular access for hemodialysis." Kidney and Blood Pressure Research 32, no. 1 (2009): 59-66. https://doi.org/10.1159/000205522
Quicken, Sjeng, Yeshi de Bruin, Barend Mees, Jan Tordoir, Tammo Delhaas, and Wouter Huberts. "Computational study on the haemodynamic and mechanical performance of electrospun polyurethane dialysis grafts." Biomechanics and modeling in mechanobiology 19, no. 2 (2020): 713-722. https://doi.org/10.1007/s10237-019-01242-1
Javadzadegan, Ashkan, Andy SC Yong, Michael Chang, Austin CC Ng, John Yiannikas, Martin KC Ng, Masud Behnia, and Leonard Kritharides. "Flow recirculation zone length and shear rate are differentially affected by stenosis severity in human coronary arteries." American Journal of Physiology-Heart and Circulatory Physiology 304, no. 4 (2013): H559-H566. https://doi.org/10.1152/ajpheart.00428.2012
Ko, T. H., Kuen Ting, and H. C. Yeh. "Numerical investigation on flow fields in partially stenosed artery with complete bypass graft: An in vitro study." International communications in heat and mass transfer 34, no. 6 (2007): 713-727. https://doi.org/10.1016/j.icheatmasstransfer.2007.03.010
Sunamura, M., H. Ishibashi, and T. Karino. "Flow patterns and preferred sites of intimal thickening in bypass-grafted arteries." International Angiology: a Journal of the International Union of Angiology 31, no. 2 (2012): 187-197.
Reininger, Armin J., Ulrich Heinzmann, Cornelia B. Reininger, Peter Friedrich, and Laurenz J. Wurzinger. "Flow mediated fibrin thrombus formation in an endothelium-lined model of arterial branching." Thrombosis Research 74, no. 6 (1994): 629-641. https://doi.org/10.1016/0049-3848(94)90219-4
Ghista, Dhanjoo N., and Foad Kabinejadian. "Coronary artery bypass grafting hemodynamics and anastomosis design: a biomedical engineering review." Biomedical engineering online 12 (2013): 1-28. https://doi.org/10.1186/1475-925X-12-129
Keynton, Robert S., S. E. Rittgers, and M. C. S. Shu. "The effect of angle and flow rate upon hemodynamics in distal vascular graft anastomoses: an in vitro model study." (1991): 458-463. https://doi.org/10.1115/1.2895427
Staalsen, Niels-Henrik, Michael Ulrich, Jens Winther, Erik Morre Pedersen, Thien How, and Hans Nygaard. "The anastomosis angle does change the flow fields at vascular end-to-side anastomoses in vivo." Journal of vascular surgery 21, no. 3 (1995): 460-471. https://doi.org/10.1016/S0741-5214(95)70288-1
Ruvolo, Giovanni, Calogera Pisano, Fabio Bertoldo, Marco Russo, Roberto Verzicco, and Paolo Nardi. "A mathematical model to evaluate hemodynamic effects of the graft anastomosis in coronary surgery." Kardiochirurgia i Torakochirurgia Polska/Polish Journal of Thoracic and Cardiovascular Surgery 16, no. 2 (2019): 106-108. https://doi.org/10.5114/kitp.2019.86366
Apan, Jhon Jasper, Lemmuel Tayo, and Jaime Honra. "Numerical Investigation of the Relationship between Anastomosis Angle and Hemodynamics in Ridged Spiral Flow Bypass Grafts." Applied Sciences 13, no. 6 (2023): 4046. https://doi.org/10.3390/app13064046